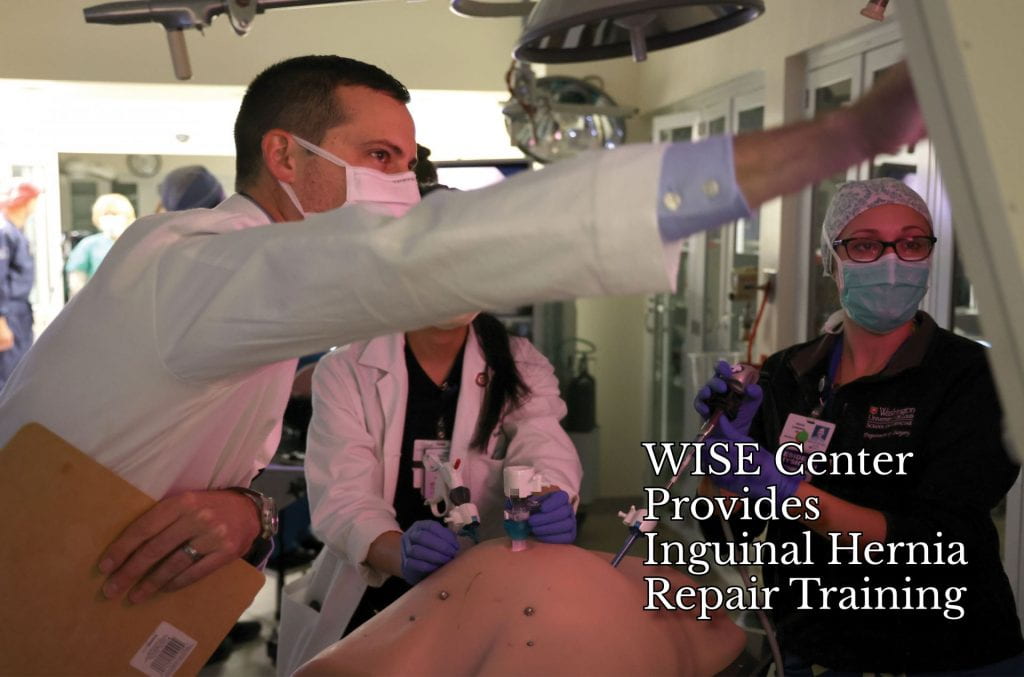
Residents recently had the opportunity to practice their surgical skills on real-tissue simulators at the Washington University Institute for Surgical Education (WISE) Center. The WISE Center and industry partner KindHeart provided residents a tissue model for inguinal hernia repair training.
Inguinal hernias, which occur in the groin, are the most common type of hernia. Surgeons at the School of Medicine repair inguinal hernias through either traditional open surgery or minimally invasive surgery, depending on what is best for the person. Early training in inguinal hernia repair using real tissue helps prepare residents who plan to specialize in such surgeries following their training, and provides important simulated experience to all surgical trainees.
Simulation training typically relies on one of two models: tissue models and non-tissue models. There are pros and cons to each. Practicing surgical skills on actual tissue gives the trainee the closest experience to an actual procedure, while non-tissue models are easily accessible and cost-effective.
“Tissue has elasticity. There is bleeding for the surgeon to manage. With real tissue, you can practice using energy devices,” WISE Director Michael Awad, MD, PhD, says. “The downside is that tissue models are a large resource, which involves costs and logistical challenges.”
Non-tissue models, such as foam rubber and cardboard boxes are excellent for practicing suturing skills and other fundamentals. These are inexpensive, easy to acquire and come at a low cost to the simulation center. The cons are that these non-tissue models do not have the same elasticity as real tissue and cannot be used for practice with energy devices.
“The KindHeart model is in a sweet spot between those two options,” Awad says. “It is tissue from an animal model, so it has the elasticity and conduction of real tissue. It replicates the anatomy more closely than a rubber model might. The cost is lower than with other, larger tissue models, and the size is convenient for working in the simulation center.”
This porcine comes in a cassette so that it can be removed and swapped with new tissue when needed. The cassette includes the inguinal ligament, inferior epigastric artery, Coopers ligament and testicular vessels. Simulated tasks include plane dissection, hernia sac reduction, mesh placement and closure. To simulate the experience of a real operation, the WISE Center housed the cassette in an abdominal trainer.
“Junior residents are glad to have the hands-on experience,” WISE Coordinator Karen Schubert says. “One of the main things I see is that the experience of senior residents training junior residents in these labs benefits everyone. It builds camaraderie among them, and the senior residents are grateful for the teaching opportunity.”